- 🫀 What Is a Heart Attack?
- 🩻 What Is Chronic Coronary Artery Disease?
- ⚠️ Why Does Coronary Artery Disease Matter?
- 🧠 What Are the Symptoms of a Heart Attack?
- 🩺 How Are Heart Attacks Treated?
- 💊 Common Medications for CAD and Heart Attacks
- 🧠 What Can You Do to Live Well With CAD?
- 💬 Frequently Asked Questions
- ✅ Final Takeaway
- 🔗 Learn More
🫀 What Is a Heart Attack?
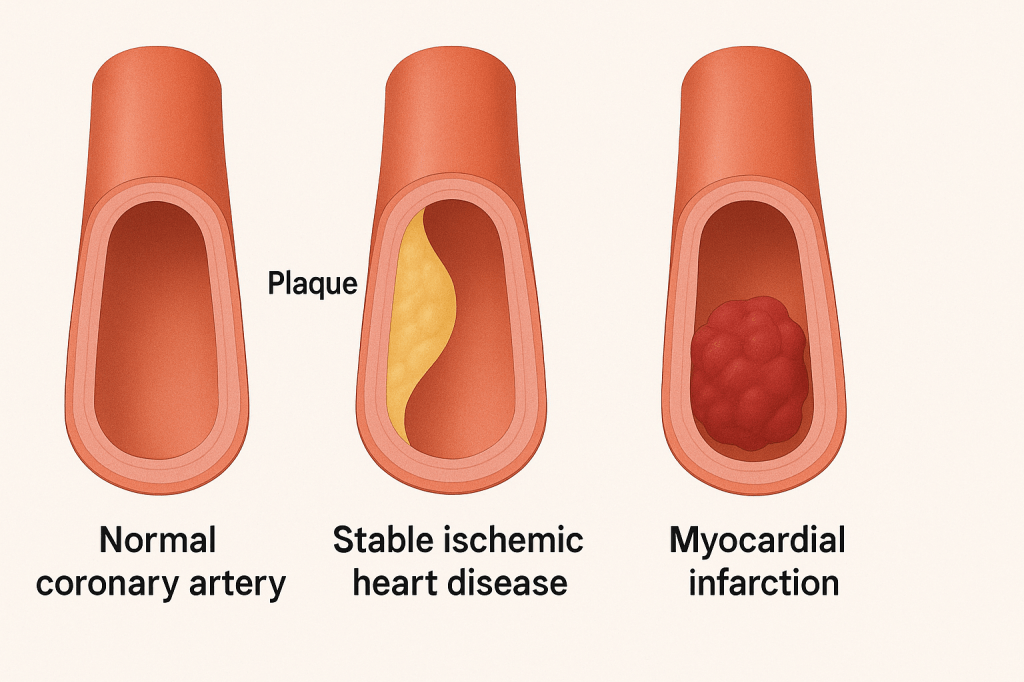
A heart attack (myocardial infarction) happens when a blood clot suddenly blocks blood flow to part of the heart muscle. Without oxygen, the affected heart tissue begins to die.
This usually occurs due to coronary artery disease (CAD) — a buildup of plaque (fat, cholesterol, and calcium) in the arteries that supply blood to the heart.
🩻 What Is Chronic Coronary Artery Disease?
Chronic coronary artery disease (also called stable ischemic heart disease) refers to a condition where heart arteries (coronary arteries) are narrowed, but not necessarily completely blocked. Blood flow to parts of the heart is reduced, which can cause symptoms at rest or especially during physical activity or stress.
This condition develops over years, and while it may not cause a heart attack right away, it increases long-term risk of cardiovascular events.
💡 Common Symptoms of Chronic CAD:
- Chest discomfort or tightness with exertion (known as angina)
- Shortness of breath with activity
- Fatigue
- Symptoms that improve with rest or nitroglycerin
Important: If symptoms change suddenly (e.g. chest pain at rest), it may indicate an emergency.
🧭 How Is Chronic CAD Diagnosed?
- Stress testing (with ECG, echocardiogram, or nuclear imaging)
- CT angiography or coronary angiogram
- Blood tests to assess cardiac risk factors
- Echocardiogram to check heart function
🛡️ How Is Chronic CAD Managed?
Goal: Prevent heart attacks, reduce symptoms, and improve quality of life.
Lifestyle:
- Heart-healthy diet (Mediterranean/DASH)
- Regular physical activity (if deemed safe by your medical team)
- Smoking cessation
- Weight management
- Stress reduction
Medications:
- Aspirin (or other antiplatelet): Prevent clots
- Statins: Lower LDL, stabilize plaques, and reduce inflammation
- Beta-blockers: Reduce angina and blood pressure
- ACE inhibitors/ARBs: Reduce blood pressure, prevents heart attacks, stabilize plaques
- Nitroglycerin (spray or tablet): For symptom relief during angina
- SGLT2 inhibitors or GLP-1 receptor agonists in patients with diabetes or obesity
In some cases, procedures like angioplasty and stenting or bypass surgery are used if symptoms persist or if blood flow is severely restricted.
⚠️ Why Does Coronary Artery Disease Matter?
Coronary artery disease, whether stable or unstable, is the #1 cause of death worldwide. It can lead to:
- Heart attack
- Heart failure
- Arrhythmias
- Sudden cardiac death
But the condition is treatable and manageable, especially when caught early.
🧠 What Are the Symptoms of a Heart Attack?
- Chest pressure, tightness, burning, or heaviness
- Pain that spreads to jaw, arm, neck, or back
- Shortness of breath
- Nausea, lightheadedness, or cold sweats
- Fatigue or dizziness
Women, older adults, and people with diabetes may have less typical symptoms. If in doubt, you should call 911. Rapid treatment of heart attacks is essential – time is muscle!
🩺 How Are Heart Attacks Treated?
In Hospital (Acute Management):
- Aspirin and other blood thinners
- Statins to stabilize plaques and rapidly lower cholesterol
- Beta blockers to prevent arrhythmias, improve heart function, and reduce strain on the heart
- ACE inhibitors/ARBs to improve heart function and reduce blood pressure
- Nitroglycerin for chest pain
- Emergency angioplasty and stenting (PCI)
- Sometimes: coronary artery bypass surgery
After Discharge:
- Daily medications (usually some medications should continue for life)
- Cardiac rehabilitation
- Lifestyle modifications
- Ongoing monitoring and support
💊 Common Medications for CAD and Heart Attacks
| Medication Class | Example(s) | What it Does | Common & Important Side Effects |
|---|---|---|---|
| Antiplatelet agents | Aspirin, Clopidogrel | Prevents blood clots | Stomach irritation, bleeding, bruising |
| Statins | Atorvastatin, Rosuvastatin | Lowers LDL cholesterol and stabilizes plaque | Muscle aches, liver enzyme changes, rarely rhabdomyolysis |
| Beta-blockers | Metoprolol, Bisoprolol | Slows heart rate, lowers blood pressure, reduces heart’s oxygen demand | Fatigue, low heart rate, lightheadedness, low mood/libido |
| ACE inhibitors / ARBs | Ramipril, Perindopril / Valsartan | Lowers blood pressure, protects heart and kidneys | Cough (ACEi), dizziness, high potassium, angioedema (rare) |
| Nitrates | Nitroglycerin (short-acting or patch) | Relieves chest pain by dilating blood vessels | Headache, low blood pressure, flushing |
| Calcium channel blockers | Amlodipine, Diltiazem | Lowers blood pressure, reduces angina | Swelling in legs, dizziness, constipation, flushing |
| SGLT2 inhibitors (if diabetic or heart failure) | Empagliflozin, Dapagliflozin | Lowers blood sugar, reduces heart failure risk | Genital infections, urination, ketoacidosis (rare) |
These medications are often used long-term, even if you feel well.
🧠 What Can You Do to Live Well With CAD?
- Stay physically active (as advised)
- Eat a heart-healthy diet
- Take medications as prescribed
- Don’t smoke — seek support to quit or reduce as much as possible
- Monitor blood pressure, cholesterol, and blood sugar
- Attend cardiac rehab (if offered)
- Manage stress
- Manage mental health (depression, anxiety, and PTSD are common after heart attacks – discuss with your physician if you notice changes in your mood).
💬 Many people with chronic CAD live long and active lives with the right treatment and lifestyle changes.
💬 Frequently Asked Questions
❓ Can I exercise with coronary artery disease?
Yes, and it’s encouraged! But always get guidance from your healthcare provider or cardiac rehab program.
❓ Do stents or surgery “cure” CAD?
No — they improve blood flow and relieve symptoms, but lifestyle and medications are still needed to prevent future events.
❓ Will anything reduce the amount of blockage in my coronary arteries?
Most medications and lifestyle changes don’t “remove” plaque completely, but they stabilize it, reduce inflammation, and slow or stop progression.
What helps:
- Statins (cholesterol-lowering medications) are the most effective at stabilizing plaque and reducing cardiovascular events. Some evidence shows they may even slightly shrink plaque over time if cholesterol levels are very low.
- Angioplasty with stents can physically open up narrowed blood vessels through a minimally invasive procedure through the arteries in the wrist or groin. For many people, this is a very helpful or life-saving procedure, but not all blockages benefit from angioplasty. These are often complex, patient-specific decisions. Speak to your physician if you have questions.
- Lifestyle changes (healthy diet, exercise, smoking cessation) help improve how well your arteries function, even if the plaque remains.
🩺 Key point: You don’t need to “clean out” your arteries — you need to stabilize them and reduce your heart attack risk, which modern therapies do very effectively.
❓ Can I drive or work after a heart attack?
Yes, but driving is regulated by provincial transportation authorities. In Ontario, for example, the Ministry of Transportation (MTO) has specific rules about when individuals can return to driving after a heart attack or with CAD. The rules depend on your particular heart condition, so they should be discussed with your physician.
Key points:
- For commercial drivers, restrictions are stricter. You may need longer periods off and more detailed assessments. Commercial driving includes rideshare work (e.g. Uber, Lyft).
- People with ongoing symptoms (e.g. unstable angina, uncontrolled arrhythmias, or fainting) are not permitted to drive until their condition is stabilized.
Always speak to your healthcare provider before resuming driving. They are required to report to the MTO if your condition poses a safety risk.
Driving restrictions can be very difficult to manage for many people. The MTO has created these rules to reduce the risk of serious health issues occurring while driving, which can put your life and the lives of other people at risk.
✅ Final Takeaway
Whether it’s chronic CAD or a heart attack, heart disease is serious — but manageable. With proper treatment, a healthy lifestyle, and regular follow-up, you can lower your risk and live a fulfilling life.